Think back to waiting in a doctor’s office as a child. The buzzing of fluorescent lights overhead, the smell of musty magazines on the coffee table. You may remember a stack of multicolored medical record folders behind the registration desk, which are now stored in electronic medical records (EMRs). Or you may remember an elderly patient in the waiting room who struggled to physically make it to the office, who can now receive nearly the same level of care in the comfort of their own home. Or you may recall the frustration of filling out written paperwork that you already completed for a different doctor in the same health system, but that can now be filled out in advance online and shared through the interoperability of health technology platforms.
In the not-so-distant past, health care was a different world. According to the American Academy of Family Physicians, the typical patient in America must wait three weeks for an appointment with a family medicine doctor, only to receive what historically has too often felt like a one-size-fits-all approach to their care.1 Times are changing.
As we move further into the 21st century, the health care industry is rapidly evolving, with new technologies and practices emerging every year that boast the potential to improve patient outcomes and deliver better care. However, with this rapid change comes a risk of falling behind. What once might have been considered cutting-edge innovation or a distinct competitive advantage has quickly become an industry expectation, leaving those who do not keep up at a disadvantage.
In this article, we will explore the future of health care and key trends driving this transformation. From digitization and the “Consumerization of Health care” to increased investment in geriatric services and a case study exploring precision medicine, we will examine how these once-considered novel innovations are becoming a necessity in staying ahead of the curve. While COVID-19 has accelerated the pace of change in health care, the changes we see today are part of a much larger journey, one that has been unfolding for some time.
1. How Digital Health Is Transforming Patient Care
From a health care provider’s perspective, digital health has come a long way since the mid-2000s with the enhancements of electronic health records (EHRs), support of government initiatives,2 and widespread accessibility to smartphones. The evolution of digital health has been rapid. Early solutions like wearables (e.g., fitness trackers) and mobile apps focused on basic health monitoring. As technology has progressed, so have the capabilities of digital health tools. Today, digital health encompasses a wide range of solutions including telemedicine, electronic health records, and AI-powered diagnostic tools. These tools are transforming health care delivery and improving patient outcomes.
The implications of digital health are immense. It has allowed health care providers to expand their reach using telemedicine to care for patients in remote or rural areas who may not otherwise have had access. Remote consultations have led to improved outcomes and reduced health care costs as patients can receive care without the need to travel long distances to see a specialist. Telemedicine has also been used to deliver mental health services, allowing patients to receive care in the comfort of their own homes.
Electronic health records have streamlined documentation and have made it easier to share information between providers leading to better care coordination. AI-powered diagnostic tools are helping providers make more accurate diagnoses and develop personalized treatment plans leading to improved patient outcomes. Digital health has also made it easier to manage patient care and reduce administrative workloads, allowing providers to focus on delivering high-quality, personalized care.
Digital health has the potential to transform the health care industry and improve patient outcomes. As technology continues to advance, health care providers will have even more tools at their disposal to deliver high-quality, personalized care to their patients. The future of digital health is exciting. Its potential to revolutionize health care delivery and improve patient outcomes is limitless. Health care providers and health care organizations must embrace the opportunities and challenges of digital health to provide better care for their patients.
2. How the “Consumerization of Health Care” Is Bringing Patients to the Forefront
Does it feel like health care has taken much longer to join the digital age than other industries? Amazon’s impact on e-commerce began in the late 1990s and continued to grow into the early 2000s, demonstrating the potential of online marketplaces and reinventing retail models. eBay, established in 1995, introduced the concept of online auctions showcasing the potential of new marketplaces regardless of physical proximity. And in 1998, PayPal revolutionized payment capabilities by introducing a secure and convenient way for individuals and businesses to conduct financial transactions online.
E-commerce, retail marketplaces, and payment platforms have continued to transform exponentially in response to consumer feedback and demand since their inception; yet, when we look at the health care industry, until recently, it feels like patients were encumbered by outdated, inefficient, and not user-friendly processes and interfaces that evolved at a pace unaffected by the patient experience. If the first electronic health records can be traced back to the Mayo Clinic in the 1960s, why has it taken so long for health care technology to innovate? And why have patients felt like they’ve just been along for the ride in their own health care journey?
An explanation, not unique to just the health care industry, is that it can largely be attributed to the way that the majority of health care is paid for. According to the Census Bureau, over 90 percent of Americans receive their insurance from employer-based commercial (e.g., Aetna, Blue Cross, United Health care, etc.) or government-sponsored (e.g., Medicare, Medicaid, TRICARE, VA) health plans.3 In the American health care journey, after a patient presents to a medical provider for care, their insurance company will typically pay for the services. With the paying entity of health care often being decided by their employer-issued or government-issued plan, patients have historically felt a disconnect from having a direct impact on their health care choices. This has led patients to feel like they are in the passenger seat of their health care journey with the insurance companies and health care providers sitting behind the wheel.
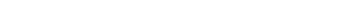
In 2019, however, a perfect storm of drivers accelerated the patient’s role in the health care journey. Between COVID-19 taking the central stage and technological innovations in wearable technologies (Internet of Things), personalization through application development, and the interoperability of technology solutions, patients began to exert more influence over how they wanted to experience care. This led to a shift of patients moving into the driver’s seat of their own health care experiences and from being viewed merely as patients, to now being viewed as consumers similar to other industries. This transformation is often referred to as the “Consumerization of Health Care.”
As health care organizations try to meet the increasing expectations of their consumers, many of whom now have a choice in health care, there is an emergence of health care technologies and services in the market. From the explosion of the digital health solutions mentioned in the previous section to the growth of retail health to the increased focus on “whole health,” consumers, providers, and payers alike are seeing a rise in new markets of health care product and service offerings driven by patient and provider demand.
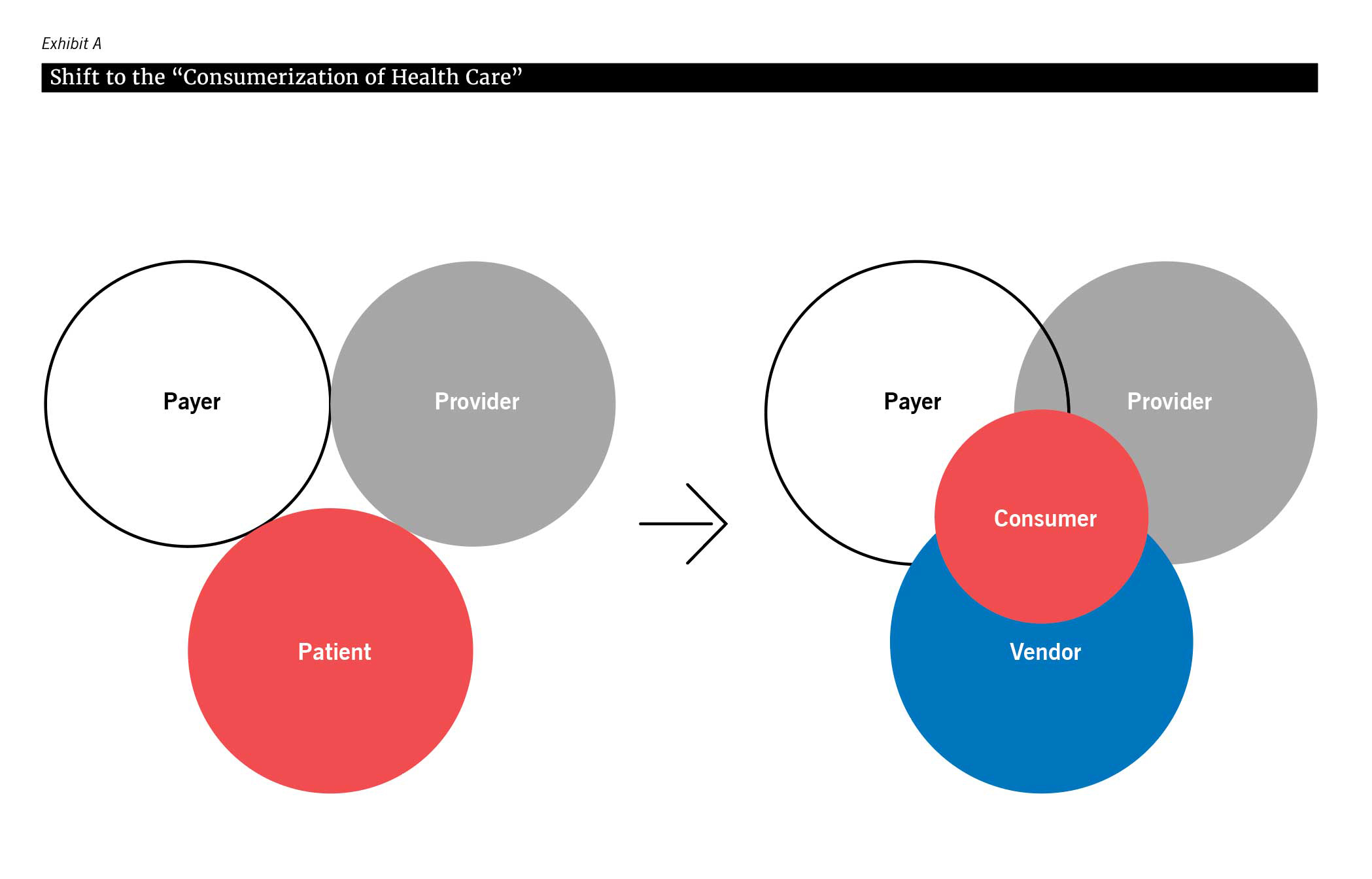
As this consumer-centric model continues in parallel with technological innovations, health care organizations are being required to balance between patient desires, what health care providers are excited about, and what health care technology and service vendors are providing (see Exhibit B). According to a KLAS Research study on patient engagement technologies, there is currently a misalignment between these three groups with the outcomes often favoring the provider rather than the consumer/patient.4 Organizations need to keep the voice of the consumer/patient top of mind in their care delivery strategy moving forward.
3. How Providers Are Preparing to Care for the Aging Population through Investments in Geriatric Care
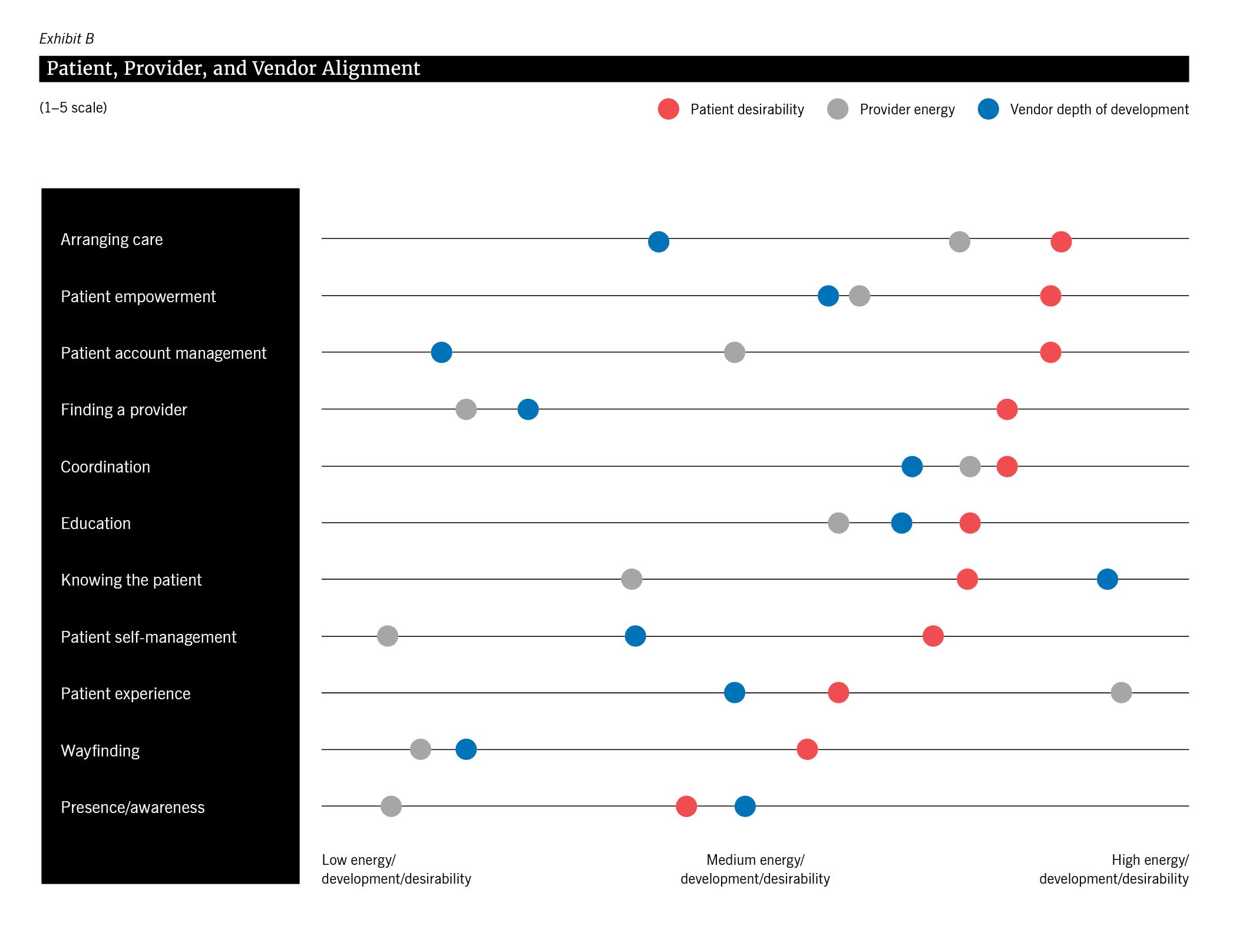
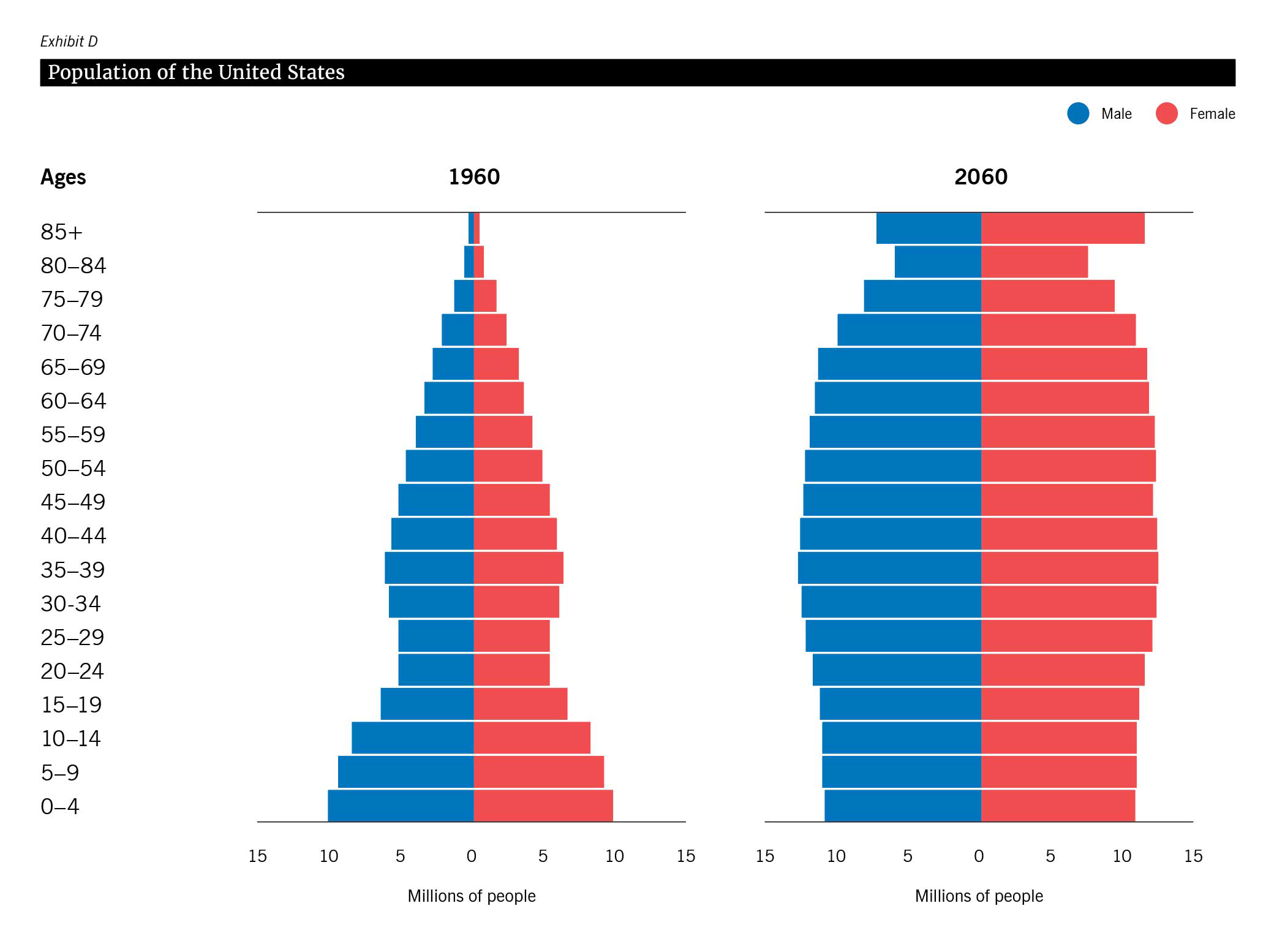
Studies show that the number of adults aged 65 and older in the United States is projected to double by 2060, accounting for over 23 percent of the population. Additionally, it is estimated that by 2030, the United States will have more adults aged 65 and older than children under 18, highlighting the significant demographic change occurring. This demographic shift, often referred to as “The Graying of America,” poses challenges and opportunities for health care systems, prompting increased investment in geriatric care.5
As the population ages, investment in quality geriatric care — including home health and hospice services — has become increasingly important. These services are designed to provide seniors with the care they need to maintain their independence and quality of life, while also allowing them to age in place.
In recent years, there has been significant innovation and investment in this space, with companies developing new technologies and services to better meet the needs of older adults. Many home health agencies now leverage technology to remotely monitor patients and deliver care more efficiently. This includes virtual visits with health care providers, medication reminders, and remote monitoring of vital signs. By using technology to connect with patients in their homes, these services can provide high-quality care while also reducing the burden on hospitals and other health care facilities.
“
It is estimated that by 2030, the United States will have more adults aged 65 and older than children under 18, highlighting the significant demographic change occurring.
Another key area of innovation in geriatric care is hospice services. Hospice care is designed to provide comfort and support for patients with terminal illnesses and their families. This can include pain management, emotional and spiritual support, and other personalized services such as music or art therapy — designed to improve the final stages of life. Interdisciplinary care teams have emerged as a vital component of comprehensive geriatric care. These teams consist of health care professionals from various disciplines who work together to address the complex needs of older adults, considering their medical, functional, emotional, and social well-being. Mental health services have also gained recognition in geriatric care, with screenings, assessments, and therapies being incorporated into more comprehensive approaches to patient care.
Further, age-friendly community initiatives are promoting aging in place, creating environments that help older adults live independently and actively in their communities. These initiatives focus on accessible infrastructure, social engagement, food delivery, transportation, and mobility support to ensure older adults can age comfortably and with dignity while maintaining their connections and participating in community life.
Organizations need to embrace and invest in technology, foster interdisciplinary collaboration, promote mental health services, and invest in the infrastructure to handle the growing demand of an increasingly aging population. These actionable steps can help improve the quality of geriatric care, enhance patient outcomes, and adapt to the changing needs of older adults.
CASE STUDY
How Cancer Treatment Is Becoming More Personalized
Precision medicine is an emerging field in health care that holds immense promise for the future of medical practice. It involves tailoring medical treatments and interventions to the individual characteristics of each patient, recognizing that each person’s genetic makeup, lifestyle, environment, and even microbiome can play a crucial role in their health and disease risk. By leveraging advanced technologies like genomics, proteomics, artificial intelligence, and data analytics, precision medicine aims to provide more personalized and targeted therapies, leading to better outcomes and reduced adverse effects. This transformative field has the potential to revolutionize how we diagnose, treat, and prevent diseases, moving away from the traditional one-size-fits-all approach to a more precise and effective model of care. As research continues to expand, precision medicine holds promise for reshaping the future of medicine and improving patient well-being on an unprecedented scale.
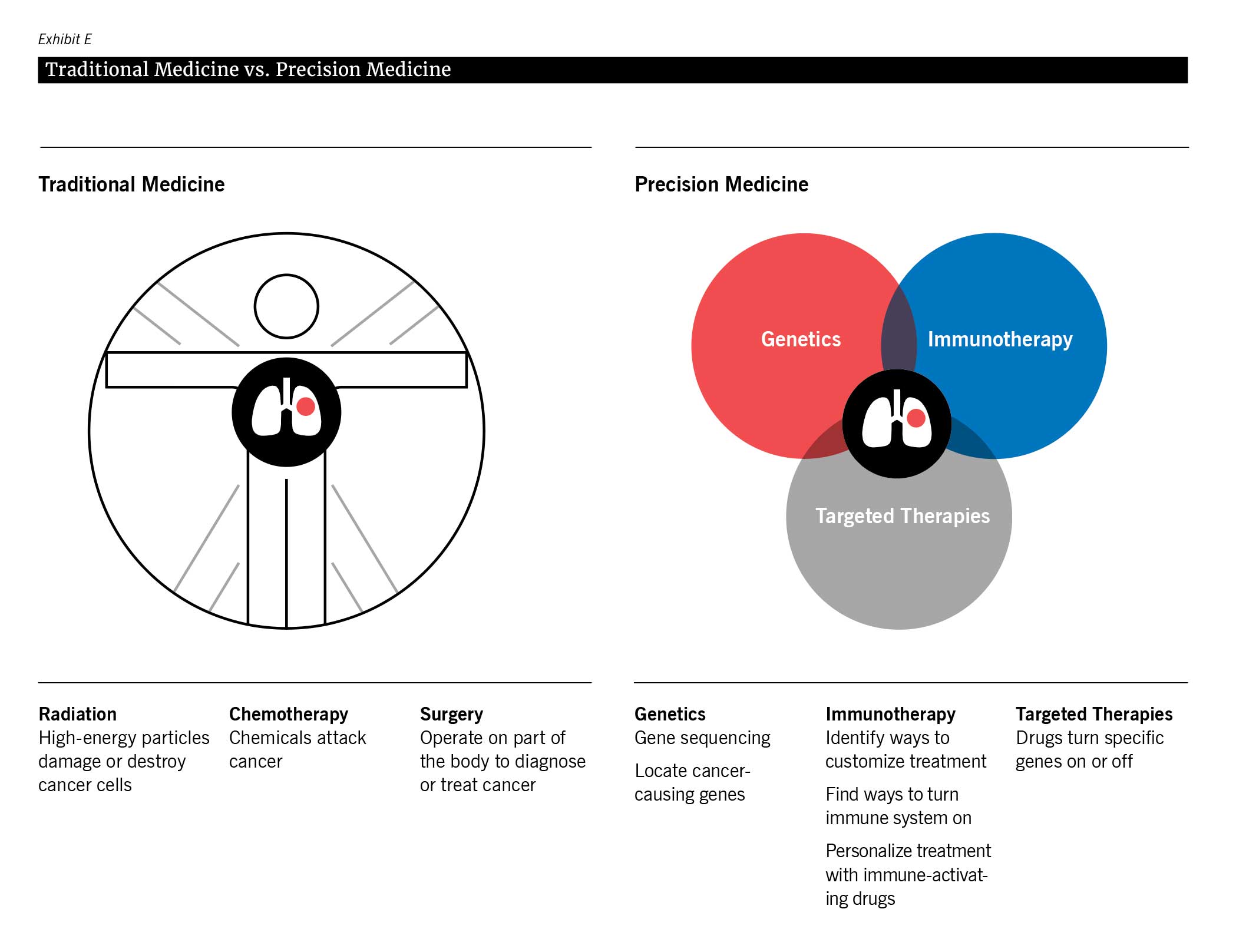
To better understand how precision medicine is changing the future, we examine precision oncology, a specific application of precision medicine related to cancer treatment, and how it offers new hope for cancer patients.
Personalized Diagnostics:
Precision oncology relies on personalized diagnostics to guide treatment decisions. By analyzing an individual’s genetic information, researchers and clinicians can identify disease markers, assess the likelihood of developing certain conditions, and predict treatment responses. In precision oncology, personalized diagnostics involves analyzing a patient’s tumor DNA, RNA, and protein expression to identify specific genetic mutations and molecular pathways driving cancer growth. These diagnostics enable more accurate diagnoses, a better understanding of cancer behavior, and the ability to tailor treatment plans to each patient’s unique characteristics. The element of time is a precious resource in an individual’s battle with cancer. Personalized diagnostics save valuable time that would otherwise have been spent in excruciatingly painful trial and error.
Targeted Therapies:
Precision medicine and precision oncology emphasize the development of targeted therapies. Traditional one-size-fits-all treatments often lack efficacy for certain patients and may cause adverse effects. However, with precision medicine, therapies can be tailored to an individual’s unique genetic profile, enhancing treatment effectiveness, and reducing side effects.
In precision oncology, targeted therapies specifically address the molecular alterations driving cancer growth. These therapies, such as tyrosine kinase inhibitors, immunotherapies, and gene therapies, provide personalized treatment options that lead to improved outcomes for cancer patients. For example, the identification of specific genetic mutations, such as the HER2 gene amplification in breast cancer, has paved the way for targeted therapies like Herceptin, which significantly improves survival rates for patients with this mutation.
The power of targeted therapies is exemplified by the groundbreaking success of immunotherapies in precision oncology. Checkpoint inhibitors, such as pembrolizumab (Keytruda), have revolutionized the treatment of advanced melanoma by blocking proteins that inhibit the immune response against cancer cells. This breakthrough has resulted in long-term remissions and even complete responses in patients who were previously considered untreatable.
Data-Driven Health Care:
Both precision medicine and precision oncology rely on extensive data analysis to guide clinical decisions. The integration and analysis of genetic data, electronic health records, and insurance records provide valuable insights. Artificial intelligence and machine learning algorithms play a crucial role in analyzing complex datasets, identifying patterns, and generating actionable insights. This data-driven approach allows for more informed diagnoses, optimized treatment strategies, and improved patient outcomes. The ongoing advancements in machine learning will continue to drive progress in precision medicine and precision oncology.
Ethical Considerations:
Precision medicine, including precision oncology, raises ethical considerations that must be addressed. Privacy concerns surrounding the collection and storage of sensitive genetic data need to be carefully managed to ensure patient trust. Equitable access to precision medicine must be prioritized to avoid exacerbating health care disparities. Transparency, informed consent, and ethical guidelines are essential to ensure that it benefits all individuals and communities.
Efforts are being made to ensure equitable access to these advanced treatments. For instance, the All of Us Research Program in the United States aims to include underrepresented populations to ensure that the benefits of precision medicine reach everyone, regardless of their socioeconomic background or ethnicity.
Challenges and the Future of Precision Medicine:
Despite the tremendous potential of precision medicine and precision oncology, several challenges lie ahead. Technological limitations, high costs, and the need for extensive infrastructure are hurdles that must be overcome for widespread implementation. The complexity of cancer genomics poses an ongoing challenge to the advancement of precision oncology. However, ongoing research and development promise to address these challenges and advance the field further. Liquid biopsies offer the speed and convenience of a blood draw in place of invasive surgery for obtaining samples and can be leveraged for early detection and ongoing monitoring.
Precision medicine, with precision oncology as a prominent subfield, holds great promise for revolutionizing health care and cancer treatment. In the context of ethical considerations, by embracing personalized diagnostics, targeted therapies, and data-driven health care, precision medicine aims to provide tailored treatments and improve patient outcomes. While challenges exist, ongoing research, technological advancements, and a commitment to equitable access and ethical practices will shape the future of precision medicine and precision oncology.
Conclusion
Health care has undergone rapid and significant transformation fueled by technological advancements and changing patient needs. The shift from traditional health care practices to digitization, AI, precision medicine, and treating an increasingly aging population has revolutionized the way health care is delivered. Patients are now consumers with their own expectations. These trends not only have the potential to improve patient outcomes but also reshape the expectations of patients and providers alike. The changes we see today are just a glimpse of what is to come. As technology advances and patients’ needs evolve, the industry must remain proactive and forward-thinking. The future of health care is now.
- https://www.aafp.org/pubs/fpm/blogs/inpractice/entry/wait-times.html
- The formation of the Office of the National Coordinator for Health Information Technology (ONC) in 2004 to promote the adoption and use of health information technology for improved healthcare delivery and the Health Information Technology for Economic and Clinical Health (HITECH) Act enacted in 2009 aimed to accelerate the adoption of electronic health records and promote the meaningful use of health information technology.
- https://www.census.gov/library/publications/
2022/demo/p60-278.html#:~:text=Of%20the%20subtypes%20of%20health,percent)%2C%20and%20VA%20and%20CHAMPVA - https://klasresearch.com/report/patient-perspectives-on-patient-engagement-technology-2020/1670
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9881650/